
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Drug/Regimen
- Long-Term Glycaemic Durability of Early Combination Therapy Strategy versus Metformin Monotherapy in Korean Patients with Newly Diagnosed Type 2 Diabetes Mellitus
- Soon-Jib Yoo, Sang-Ah Chang, Tae Seo Sohn, Hyuk-Sang Kwon, Jong Min Lee, Sungdae Moon, Pieter Proot, Päivi M Paldánius, Kun Ho Yoon
- Diabetes Metab J. 2021;45(6):954-959. Published online November 12, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0173
- 55,052 View
- 367 Download
- 3 Web of Science
- 2 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 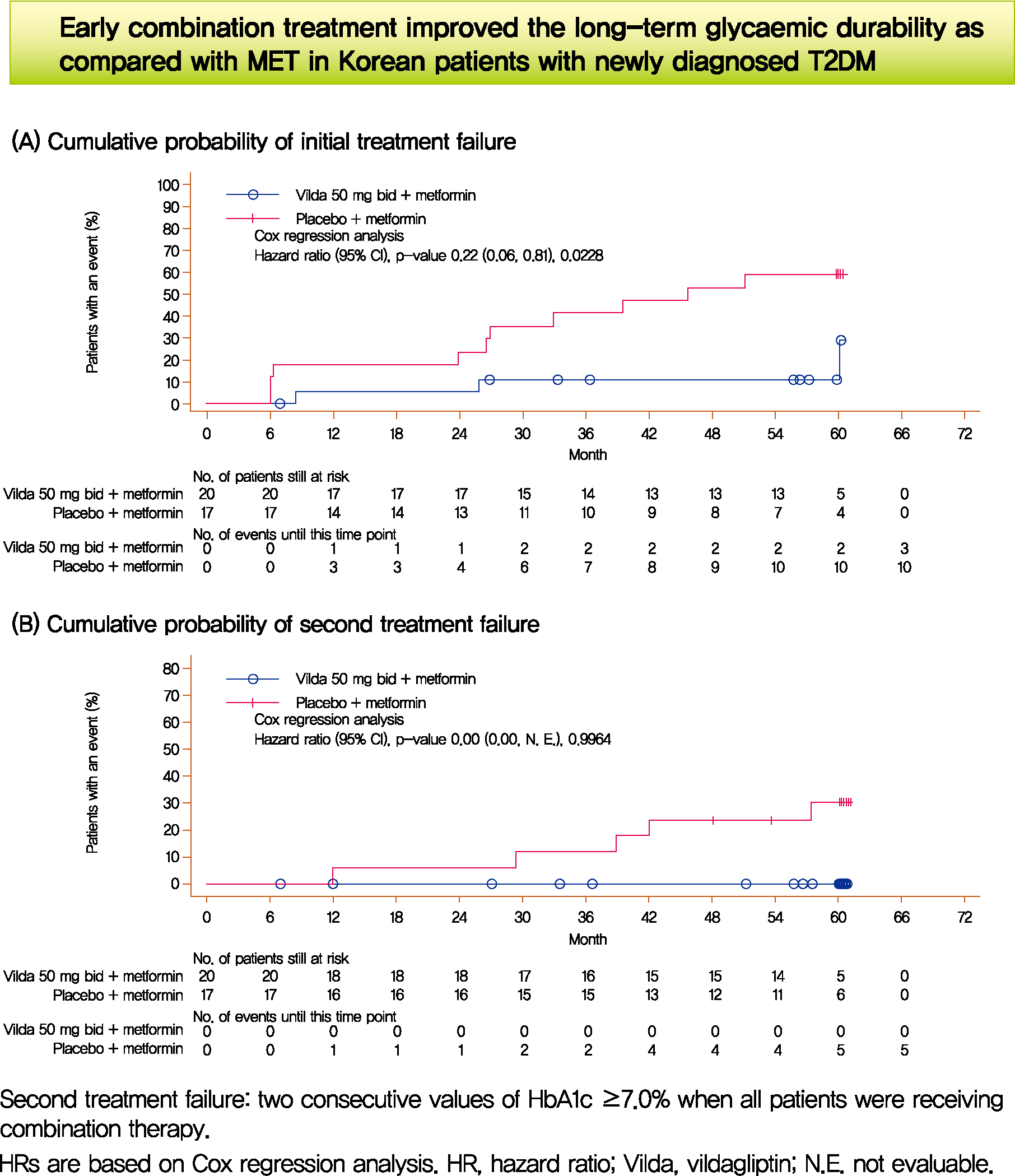
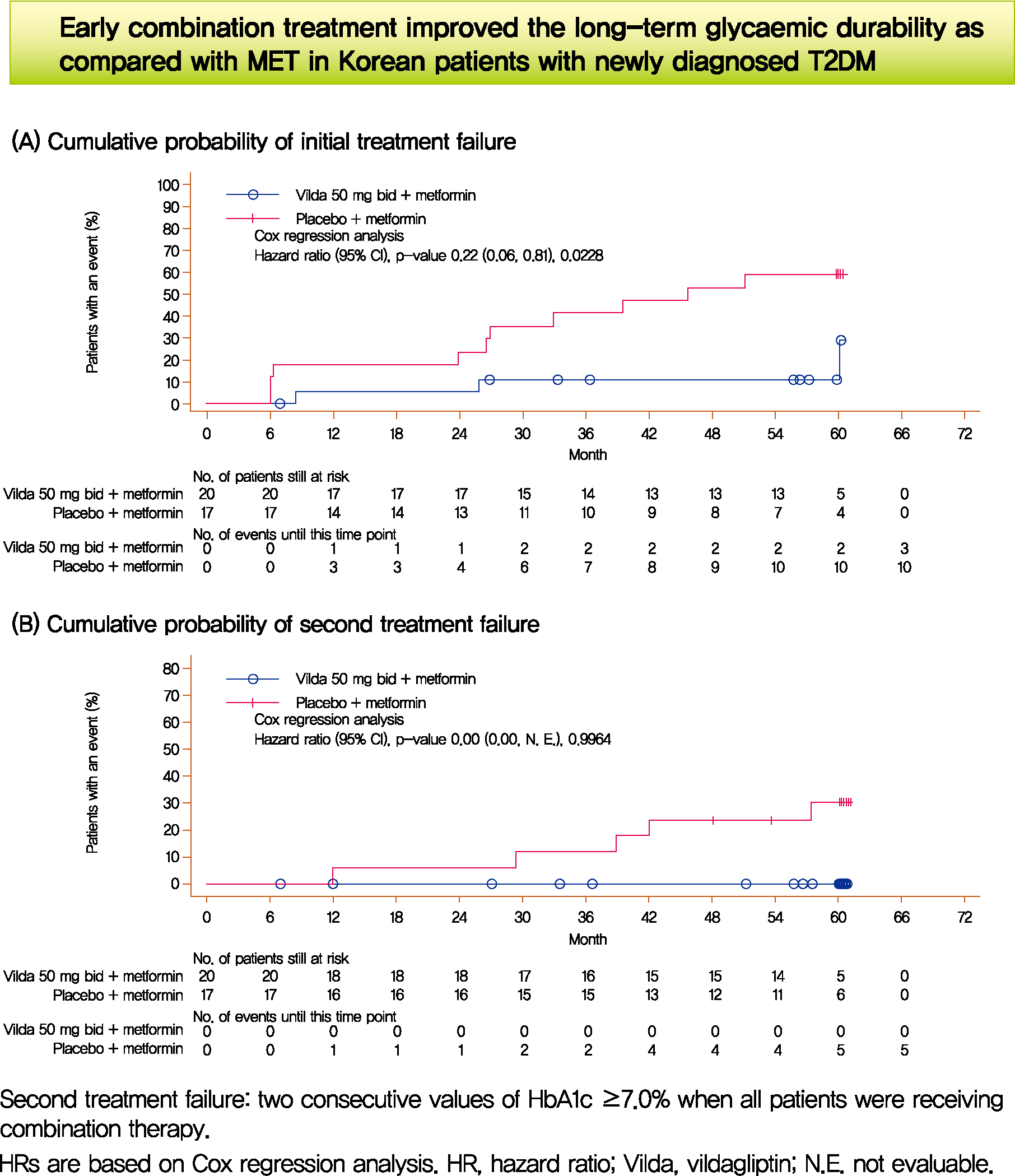
- We assessed the glycaemic durability with early combination (EC; vildagliptin+metformin [MET], n=22) versus MET monotherapy (n=17), among newly-diagnosed type 2 diabetes mellitus (T2DM) enrolled (between 2012 and 2014) in the VERIFY study from Korea (n=39). Primary endpoint was time to initial treatment failure (TF) (glycosylated hemoglobin [HbA1c] ≥7.0% at two consecutive scheduled visits after randomization [end of period 1]). Time to second TF was assessed when both groups were receiving and failing on the combination (end of period 2). With EC the risk of initial TF significantly reduced by 78% compared to MET (n=3 [15%] vs. n=10 [58.7%], P=0.0228). No secondary TF occurred in EC group versus five patients (29.4%) in MET. Patients receiving EC treatment achieved consistently lower HbA1c levels. Both treatment approaches were well tolerated with no hypoglycaemic events. In Korean patients with newly diagnosed T2DM, EC treatment significantly and consistently improved the long-term glycaemic durability as compared with MET.
-
Citations
Citations to this article as recorded by- 2023 Clinical Practice Guidelines for Diabetes Mellitus of the Korean Diabetes Association
Jong Han Choi, Kyung Ae Lee, Joon Ho Moon, Suk Chon, Dae Jung Kim, Hyun Jin Kim, Nan Hee Kim, Ji A Seo, Mee Kyoung Kim, Jeong Hyun Lim, YoonJu Song, Ye Seul Yang, Jae Hyeon Kim, You-Bin Lee, Junghyun Noh, Kyu Yeon Hur, Jong Suk Park, Sang Youl Rhee, Hae J
Diabetes & Metabolism Journal.2023; 47(5): 575. CrossRef - 2021 Clinical Practice Guidelines for Diabetes Mellitus of the Korean Diabetes Association
Kyu Yeon Hur, Min Kyong Moon, Jong Suk Park, Soo-Kyung Kim, Seung-Hwan Lee, Jae-Seung Yun, Jong Ha Baek, Junghyun Noh, Byung-Wan Lee, Tae Jung Oh, Suk Chon, Ye Seul Yang, Jang Won Son, Jong Han Choi, Kee Ho Song, Nam Hoon Kim, Sang Yong Kim, Jin Wha Kim,
Diabetes & Metabolism Journal.2021; 45(4): 461. CrossRef
- 2023 Clinical Practice Guidelines for Diabetes Mellitus of the Korean Diabetes Association
- Drug/Regimen
- Effect of Dapagliflozin as an Add-on Therapy to Insulin on the Glycemic Variability in Subjects with Type 2 Diabetes Mellitus (DIVE): A Multicenter, Placebo-Controlled, Double-Blind, Randomized Study
- Seung-Hwan Lee, Kyung-Wan Min, Byung-Wan Lee, In-Kyung Jeong, Soon-Jib Yoo, Hyuk-Sang Kwon, Yoon-Hee Choi, Kun-Ho Yoon
- Diabetes Metab J. 2021;45(3):339-348. Published online May 28, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0203

- 8,284 View
- 332 Download
- 12 Web of Science
- 15 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 
Background Glycemic variability is associated with the development of diabetic complications and hypoglycemia. However, the effect of sodium-glucose transporter 2 (SGLT2) inhibitors on glycemic variability is controversial. We aimed to examine the effect of dapagliflozin as an add-on therapy to insulin on the glycemic variability assessed using continuous glucose monitoring (CGM) in subjects with type 2 diabetes mellitus.
Methods In this multicenter, placebo-controlled, double-blind, randomized study, 84 subjects received 10 mg of dapagliflozin (
n =41) or the placebo (n =43) for 12 weeks. CGM was performed before and after treatment to compare the changes in glycemic variability measures (standard deviation [SD], mean amplitude of glycemic excursions [MAGEs]).Results At week 12, significant reductions in glycosylated hemoglobin (−0.74%±0.66% vs. 0.01%±0.65%,
P <0.001), glycated albumin (−3.94%±2.55% vs. −0.67%±2.48%,P <0.001), and CGM-derived mean glucose (−41.6±39.2 mg/dL vs. 1.1±46.2 mg/dL,P <0.001) levels were observed in the dapagliflozin group compared with the placebo group. SD and MAGE were significantly decreased in the dapagliflozin group, but not in the placebo group. However, the difference in ΔSD and ΔMAGE failed to reach statistical significance between two groups. No significant differences in the incidence of safety endpoints were observed between the two groups.Conclusion Dapagliflozin effectively decreased glucose levels, but not glucose variability, after 12 weeks of treatment in participants with type 2 diabetes mellitus receiving insulin treatment. The role of SGLT2 inhibitors in glycemic variability warrants further investigations.
-
Citations
Citations to this article as recorded by- Selective sodium-glucose cotransporter-2 inhibitors in the improvement of hemoglobin and hematocrit in patients with type 2 diabetes mellitus: a network meta-analysis
Yuanyuan Luo, Ruojing Bai, Wei Zhang, Guijun Qin
Frontiers in Endocrinology.2024;[Epub] CrossRef - Continuous Glucose Monitoring Profiles and Health Outcomes After Dapagliflozin Plus Saxagliptin vs Insulin Glargine
Donald C Simonson, Marcia A Testa, Ella Ekholm, Maxwell Su, Tina Vilsbøll, Serge A Jabbour, Marcus Lind
The Journal of Clinical Endocrinology & Metabolism.2024;[Epub] CrossRef - Impact of empagliflozin on insulin needs in patients with heart failure and diabetes: An EMPEROR‐Pooled analysis
Khawaja M. Talha, Jennifer Green, Gerasimos Filippatos, Stuart Pocock, Faiez Zannad, Martina Brueckmann, Elke Schueler, Anne Pernille Ofstad, João Pedro Ferreira, Stefan D. Anker, Javed Butler, Julio Rosenstock, Milton Packer
Diabetes, Obesity and Metabolism.2024;[Epub] CrossRef - Risk of Urinary Tract Infection in Patients with Type 2 Diabetes Mellitus Treated with Dapagliflozin: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Zhigui Zheng, Dongyuan He, Jianguo Chen, Xiaohui Xie, Yunan Lu, Binbin Wu, Xinxin Jiang
Clinical Drug Investigation.2023; 43(4): 209. CrossRef - Effect of SGLT2 Inhibitors and Metformin on Inflammatory and Prognostic
Biomarkers in Type 2 Diabetes Patients
Yang Cao, Ning Liang, Ting Liu, Jingai Fang, Xiaodong Zhang
Endocrine, Metabolic & Immune Disorders - Drug Targets.2023; 23(4): 530. CrossRef - What is Glycaemic Variability and which Pharmacological Treatment Options are Effective? A Narrative Review
Juan Miguel Huertas Cañas, Maria Alejandra Gomez Gutierrez, Andres Bedoya Ossa
European Endocrinology.2023; 19(2): 4. CrossRef - La variabilité glycémique : un facteur de risque singulier à conjuguer au pluriel
Louis Monnier, Claude Colette, Fabrice Bonnet, David Owens
Médecine des Maladies Métaboliques.2022; 16(1): 15. CrossRef - Association between Variability of Metabolic Risk Factors and Cardiometabolic Outcomes
Min Jeong Park, Kyung Mook Choi
Diabetes & Metabolism Journal.2022; 46(1): 49. CrossRef - Effect of sodium-glucose cotransporter-2 (SGLT2) inhibitors on serum urate levels in patients with and without diabetes: a systematic review and meta-regression of 43 randomized controlled trials
Alicia Swee Yan Yip, Shariel Leong, Yao Hao Teo, Yao Neng Teo, Nicholas L. X. Syn, Ray Meng See, Caitlin Fern Wee, Elliot Yeung Chong, Chi-Hang Lee, Mark Y. Chan, Tiong-Cheng Yeo, Raymond C. C. Wong, Ping Chai, Ching-Hui Sia
Therapeutic Advances in Chronic Disease.2022; 13: 204062232210835. CrossRef - Hypoglycemic agents and glycemic variability in individuals with type 2 diabetes: A systematic review and network meta-analysis
SuA Oh, Sujata Purja, Hocheol Shin, Minji Kim, Eunyoung Kim
Diabetes and Vascular Disease Research.2022; 19(3): 147916412211068. CrossRef - The Clinical Effect of Dapagliflozin in Patients with Angiographically Confirmed Coronary Artery Disease and Concomitant Type 2 Diabetes Mellitus
Yana Yu. Dzhun, Yevhen Yu. Marushko, Yanina A. Saienko, Nadiya M. Rudenko, Borys M. Mankovsky
Ukrainian Journal of Cardiovascular Surgery.2022; 30(3): 35. CrossRef - Stress-Induced Hyperglycaemia in Non-Diabetic Patients with Acute Coronary Syndrome: From Molecular Mechanisms to New Therapeutic Perspectives
Alessandro Bellis, Ciro Mauro, Emanuele Barbato, Antonio Ceriello, Antonio Cittadini, Carmine Morisco
International Journal of Molecular Sciences.2021; 22(2): 775. CrossRef - Glycemic Variability Impacted by SGLT2 Inhibitors and GLP 1 Agonists in Patients with Diabetes Mellitus: A Systematic Review and Meta-Analysis
Heeyoung Lee, Se-eun Park, Eun-Young Kim
Journal of Clinical Medicine.2021; 10(18): 4078. CrossRef - Effect of Dapagliflozin on Glycemic Variability in Patients with Type 2 Diabetes under Insulin Glargine Combined with Other Oral Hypoglycemic Drugs
Menghui Luo, Xiaocen Kong, Huiying Wang, Xiaofang Zhai, Tingting Cai, Bo Ding, Yun Hu, Ting Jing, Xiaofei Su, Huiqin Li, Jianhua Ma, Yoshifumi Saisho
Journal of Diabetes Research.2020; 2020: 1. CrossRef - Time in Range from Continuous Glucose Monitoring: A Novel Metric for Glycemic Control
Jee Hee Yoo, Jae Hyeon Kim
Diabetes & Metabolism Journal.2020; 44(6): 828. CrossRef
- Selective sodium-glucose cotransporter-2 inhibitors in the improvement of hemoglobin and hematocrit in patients with type 2 diabetes mellitus: a network meta-analysis
- Obesity and Metabolic Syndrome
-
- The Risk of Myocardial Infarction and Ischemic Stroke According to Waist Circumference in 21,749,261 Korean Adults: A Nationwide Population-Based Study
- Jung-Hwan Cho, Eun-Jung Rhee, Se-Eun Park, Hyemi Kwon, Jin-Hyung Jung, Kyung-Do Han, Yong-Gyu Park, Hye Soon Park, Yang-Hyun Kim, Soon-Jib Yoo, Won-Young Lee
- Diabetes Metab J. 2019;43(2):206-221. Published online December 27, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0039
- 5,606 View
- 102 Download
- 22 Web of Science
- 23 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background Waist circumference (WC) is a well-known obesity index that predicts cardiovascular disease (CVD). We studied the relationship between baseline WC and development of incident myocardial infarction (MI) and ischemic stroke (IS) using a nationwide population-based cohort, and evaluated if its predictability is better than body mass index (BMI).
Methods Our study included 21,749,261 Koreans over 20 years of age who underwent the Korean National Health Screening between 2009 and 2012. The occurrence of MI or IS was investigated until the end of 2015 using National Health Insurance Service data.
Results A total of 127,289 and 181,637 subjects were newly diagnosed with MI and IS. The incidence rate and hazard ratio of MI and IS increased linearly as the WC level increased, regardless of adjustment for BMI. When the analyses were performed according to 11 groups of WC, the lowest risk of MI was found in subjects with WC of 70 to 74.9 and 65 to 69.9 cm in male and female, and the lowest risk of IS in subjects with WC of 65 to 69.9 and 60 to 64.9 cm in male and female, respectively. WC showed a better ability to predict CVD than BMI with smaller Akaike information criterion. The optimal WC cutoffs were 84/78 cm for male/female for predicting MI, and 85/78 cm for male/female for predicting IS.
Conclusion WC had a significant linear relationship with the risk of MI and IS and the risk began to increase from a WC that was lower than expected.
-
Citations
Citations to this article as recorded by- Usefulness of New Criteria for Metabolic Syndrome Optimized for Prediction of Cardiovascular Diseases in Japanese
Yurie Yamazaki, Kazuya Fujihara, Takaaki Sato, Mayuko Harada Yamada, Yuta Yaguchi, Yasuhiro Matsubayashi, Takaho Yamada, Satoru Kodama, Kiminori Kato, Hitoshi Shimano, Hirohito Sone
Journal of Atherosclerosis and Thrombosis.2024; 31(4): 382. CrossRef - Association between body composition and subsequent cardiovascular diseases among 5-year breast cancer survivors
Ji Soo Kim, Jihun Song, Seulggie Choi, Sung Min Kim, Young Jun Park, Sun Jae Park, Yoosun Cho, Yun Hwan Oh, Seogsong Jeong, Kyae Hyung Kim, Sang Min Park
Nutrition, Metabolism and Cardiovascular Diseases.2024;[Epub] CrossRef - Body mass index, waist circumference and cardiovascular diseases in transitional ages (40 and 66 years)
Jung Eun Yoo, Kyungdo Han, Jin‐Hyung Jung, Yang‐Im Hur, Yang Hyun Kim, Eun Sook Kim, Jang Won Son, Eun‐Jung Rhee, Won‐Young Lee, Ga Eun Nam
Journal of Cachexia, Sarcopenia and Muscle.2023; 14(1): 369. CrossRef - Risk factors for stroke among anthropometric indices and lipid profiles in the Korean population: a large-scale cross-sectional study
Mi Hong Yim, Young Ju Jeon, Bum Ju Lee
Scientific Reports.2023;[Epub] CrossRef - Big Data Research in the Field of Endocrine Diseases Using the Korean National Health Information Database
Sun Wook Cho, Jung Hee Kim, Han Seok Choi, Hwa Young Ahn, Mee Kyoung Kim, Eun Jung Rhee
Endocrinology and Metabolism.2023; 38(1): 10. CrossRef - Research on obesity using the National Health Information Database: recent trends
Eun-Jung Rhee
Cardiovascular Prevention and Pharmacotherapy.2023; 5(2): 35. CrossRef - Association between the weight-adjusted waist index and stroke: a cross-sectional study
Jiayi Ye, Yanjie Hu, Xinrong Chen, Zhe Yin, Xingzhu Yuan, Liping Huang, Ka Li
BMC Public Health.2023;[Epub] CrossRef - Increased risk of ischemic stroke associated with elevated gamma-glutamyl transferase level in adult cancer survivors: a population-based cohort study
Kyuwoong Kim, Hyeyun Jung, Edvige Di Giovanna, Tae Joon Jun, Young-Hak Kim
Scientific Reports.2023;[Epub] CrossRef - Changes in body composition and subsequent cardiovascular disease risk among 5-year breast cancer survivors
Ji Soo Kim, Jihun Song, Seulggie Choi, Sang Min Park
Frontiers in Cardiovascular Medicine.2023;[Epub] CrossRef - Association between Stroke and Abdominal Obesity in the Middle-Aged and Elderly Korean Population: KNHANES Data from 2011–2019
Jong Yeon Kim, Sung Min Cho, Youngmin Yoo, Taesic Lee, Jong Koo Kim
International Journal of Environmental Research and Public Health.2022; 19(10): 6140. CrossRef - Prevalence of metabolic syndrome and related factors in a large sample of antipsychotic naïve patients with first-episode psychosis: Baseline results from the PAFIP cohort
Nathalia Garrido-Torres, Miguel Ruiz-Veguilla, Luis Alameda, Manuel Canal-Rivero, María Juncal Ruiz, Marcos Gómez-Revuelta, Rosa Ayesa-Arriola, Ana Rubio-García, Benedicto Crespo-Facorro, Javier Vázquez-Bourgon
Schizophrenia Research.2022; 246: 277. CrossRef - Development and validation of risk prediction models for stroke and mortality among patients with type 2 diabetes in northern China
X. Shao, H. Liu, F. Hou, Y. Bai, Z. Cui, Y. Lin, X. Jiang, P. Bai, Y. Wang, Y. Zhang, C. Lu, H. Liu, S. Zhou, P. Yu
Journal of Endocrinological Investigation.2022; 46(2): 271. CrossRef - Neck circumference for predicting the occurrence of future cardiovascular events: A 7.6-year longitudinal study
Tingting Hu, Yun Shen, Weijie Cao, Yiting Xu, Yufei Wang, Xiaojing Ma, Yuqian Bao
Nutrition, Metabolism and Cardiovascular Diseases.2022; 32(12): 2830. CrossRef - A prospective study of waist circumference trajectories and incident cardiovascular disease in China: the Kailuan Cohort Study
Liang Wang, Yujin Lee, Yuntao Wu, Xinyuan Zhang, Cheng Jin, Zhe Huang, Yixin Wang, Zhiyi Wang, Penny Kris-Etherton, Shouling Wu, Xiang Gao
The American Journal of Clinical Nutrition.2021; 113(2): 338. CrossRef - The Repeatedly Elevated Fatty Liver Index Is Associated With Increased Mortality: A Population-Based Cohort Study
Chang-Hoon Lee, Kyung-Do Han, Da Hye Kim, Min-Sun Kwak
Frontiers in Endocrinology.2021;[Epub] CrossRef - Obesity Degree and Glycemic Status: Factors That Should Be Considered in Heart Failure
Hye Soon Kim
Diabetes & Metabolism Journal.2020; 44(4): 529. CrossRef - Exposure-weighted scoring for metabolic syndrome and the risk of myocardial infarction and stroke: a nationwide population-based study
Eun Young Lee, Kyungdo Han, Da Hye Kim, Yong-Moon Park, Hyuk-Sang Kwon, Kun-Ho Yoon, Mee Kyoung Kim, Seung-Hwan Lee
Cardiovascular Diabetology.2020;[Epub] CrossRef - Predicting the Development of Myocardial Infarction in Middle-Aged Adults with Type 2 Diabetes: A Risk Model Generated from a Nationwide Population-Based Cohort Study in Korea
Seung-Hwan Lee, Kyungdo Han, Hun-Sung Kim, Jae-Hyoung Cho, Kun-Ho Yoon, Mee Kyoung Kim
Endocrinology and Metabolism.2020; 35(3): 636. CrossRef - Obesity Fact Sheet in Korea, 2018: Data Focusing on Waist Circumference and Obesity-Related Comorbidities
Ga Eun Nam, Yang-Hyun Kim, Kyungdo Han, Jin-Hyung Jung, Yong Gyu Park, Kwan-Woo Lee, Eun-Jung Rhee, Jang Won Son, Seong-Su Lee, Hyuk-Sang Kwon, Won-Young Lee, Soon Jib Yoo
Journal of Obesity & Metabolic Syndrome.2019; 28(4): 236. CrossRef - Simply the Best: Anthropometric Indices for Predicting Cardiovascular Disease
Jie-Eun Lee
Diabetes & Metabolism Journal.2019; 43(2): 156. CrossRef - Association and Interaction Analysis of Lipid Accumulation Product with Impaired Fasting Glucose Risk: A Cross-Sectional Survey
Jian Song, Xue Chen, Yuhong Jiang, Jing Mi, Yuyuan Zhang, Yingying Zhao, Xuesen Wu, Huaiquan Gao
Journal of Diabetes Research.2019; 2019: 1. CrossRef - Letter: Association of Z-Score of the Log-Transformed A Body Shape Index with Cardiovascular Disease in People Who Are Obese but Metabolically Healthy: The Korea National Health and Nutrition Examination Survey 2007-2010 (J Obes Metab Syndr 2018;27:158-65
Eun-Jung Rhee
Journal of Obesity & Metabolic Syndrome.2019; 28(2): 139. CrossRef - Response: The Differential Association between Muscle Strength and Diabetes Mellitus According to the Presence or Absence of Obesity (J Obes Metab Syndr 2019;28:46-52)
Bo Kyung Koo
Journal of Obesity & Metabolic Syndrome.2019; 28(4): 297. CrossRef
- Usefulness of New Criteria for Metabolic Syndrome Optimized for Prediction of Cardiovascular Diseases in Japanese

 KDA
KDA
 First
First Prev
Prev





